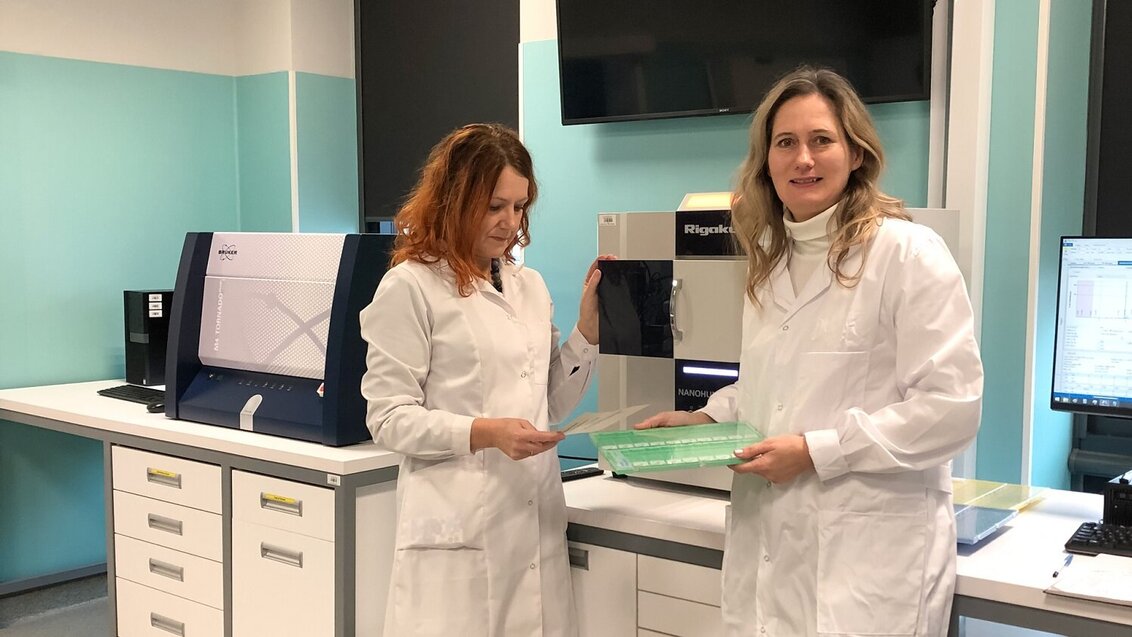
Dr Magdalena Szczerbowska-Boruchowska (on the left) and Dr Agata Ziomber-Lisiak, M.D., (on the right) in the X-ray fluorescence laboratory of the Faculty of Physics and Applied Computer Science at the AGH University. Photo by Beata Ostachowicz
Scientists from two Krakow universities joined their forces to find markers of early obesity. The results of the research by Dr Magdalena Szczerbowska-Boruchowska, associate professor from the Department of Medical Physics and Biophysics at the AGH University, and Dr Agata Ziomber-Lisiak, M.D., from the Department of Pathophysiology of the Jagiellonian University Collegium Medicum, suggest that measuring the level of one of the trace elements present in the tissues, namely rubidium, can facilitate diagnosing obesity in the future.
“The sheer awareness that this state shortens life without evident “proofs” of disorders is often insufficient for the sick person to undertake actions, as the consequences are too distant,” claimed Dr Agata Ziomber-Lisiak, M.D., on the necessity to seek precise obesity indicators.
While it may seem that a glance of the trained eye or a simple weight measurement is enough to diagnose obesity, the disease is actually much more nuanced. What all its forms have in common is a high health risk – it can shorten life by up to 10 years.
The issue of invisible kilograms
One of the groups of people struggling with obesity are those with excessive body fatness, and the disease negatively affects their metabolism, leading to complications such as hypertension and insulin resistance. In people with apparent obesity, the simplest indicator of the body’s increased risk of adverse changes associated with obesity is the BMI, or Body Mass Index. It is calculated by dividing the body mass by the square of the body height.
Although for a large group of adults this indicator is important for initial assessment, its value within the normal range does not guarantee that a person will not develop symptoms of the metabolic syndrome (including hyperglycaemia, type 2 diabetes, hypertension, and dyslipidaemia).
Due to in-depth imaging, it has been found that this syndrome also occurs in people who have a normal BMI but have a significant amount of visceral fat surrounding internal organs. Since in their case the changes are not visible on the outside of the body, and the primary indicator fails to recognise them, such people may not suspect that obesity concerns them. Until they are aware of that, they cannot undertake treatment and preventive measures, and their health continues to deteriorate.
The BMI index also fails in case of athletic people, in whom muscles (heavier than fat) account for a large proportion of total body weight, and in children, who have different body proportions at different periods of development, the classical formula for calculating BMI gives a false result. Therefore, the interpretation of the results is more complicated and requires the use of percentile grids. In addition, even in visibly obese people, this index does not inform about the distribution of excess body fat, and the effects of fat accumulation may depend on it.
The accumulation of fat around the abdomen is particularly dangerous. Adipose tissue accumulated there in a particular way (more so than adipose tissue found on the buttocks or thighs) disrupts hormonal and metabolic balance, leading to the development of type 2 diabetes and cardiovascular diseases. Specialised imaging methods can be used to diagnose abdominal obesity, but it is expensive and time-consuming, which makes it not widely used.
Also available are obesity markers based on biological samples, but they detect mainly metabolic disorders, and in some obese people such disorders do not occur. Meanwhile, as shown by studies, such individuals still face higher morbidity and mortality than the general population. Unfortunately, it is not yet entirely clear what this difference results from.
Despite the availability of commonly used indicators and obesity markers, there is still a need for more of them that would have even higher efficacy, allow early diagnosis of the disease, and make the patient aware of the need for treatment before the disease leads to serious changes in their body. At the same time, the work on them may allow a better understanding of the mechanisms behind the disorders associated with the disease.
Trace elements indicate problems
Dr Agata Ziomber-Lisiak and Dr Magdalena Szczerbowska-Boruchowska saw an opportunity to find markers of obesity in trace elements present in tissues. These elements are necessary for the proper functioning of the body, as they are responsible for building processes, enzymatic reactions, energy metabolism, and conduction of electrical impulses, i.e. basic body processes. So while the biochemical mechanism for the development of obesity is not fully understood, the effects of the disease indicate that it affects these basic tissue processes. There have already been preliminary reports of obesity-induced changes in trace element levels in hair or serum. Taking this into account, the researchers deduced that trace element levels could serve as a marker of early obesity – a substance whose level could inform of the presence of a specific condition in the body.
The tests were performed on rats. First, they were randomly assigned to two groups – for seven and a half weeks individuals in one group were given food with a higher caloric content than animals in the other group. That much was enough to observe the effect of diet on fat gain in both groups.
It is assumed that seven weeks of a high-fat diet is long enough for processes to occur in the rats' bodies that correspond to those of obese people. The material for analysis in this study was taken not only from tissues associated with obesity-related changes (i.e., liver, skeletal muscles, kidney, and adipose tissue), but also from the external ear. The possibility of assessing the condition of the body on the basis of such readily available tissue as that taken from the ear makes us optimistic about the chances of clinical trials and, in the future, the widespread use of this method as a diagnostic tool. If taking a sample for testing is easy and minimally invasive, people will be more willing to undergo the procedure, thereby increasing the chances of detecting a problem before suffering serious consequences.
The Total Reflection X-Ray Fluorescence (TXRF) technique was used to study the elemental composition. Its undisputable advantage is the ability to determine multiple elements at once, so the scientists did not have to type out potential marker candidates, but could study many of them and their interrelationships. In addition, the method is also extremely sensitive, it can detect elements as low as micrograms per kilogram, so it is well suited for the study of biological materials in which trace elements are present at very low concentration levels.
Analyses were carried out using standard statistical methods but also using advanced data mining techniques.
“The principal component analysis (PCA) we used allowed us to show that just based on the full, measured elemental composition of tissues taken from obese and non-obese individuals, we are able to determine the experimental group of each individual, to indicate which elements or parameters contribute to this distinction, as well as to learn about the interrelationships between elements. This very clear distinction of groups observed in the PCA was also confirmed by the HCA, cluster analysis. Furthermore, by incorporating the discriminant analysis, it was possible to obtain information on which elements differentiate the studied groups the most. Such an analysis allowed for determining potassium, iron, bromium, and rubid as potential chemical obesity markers. Finally, the analysis of ROC curves we used in the study made it possible to conclude that of all the elements determined, it is rubidium that shows the highest predictive efficacy," says Magdalena Szczerbowska-Boruchowska, associate professor at the AGH University, about the work of her team.
The AGH University team engaged in the research on obesity; from the left: Dr Kaja Piana, Associate Professor Magdalena Szczerbowska-Boruchowska, Dr Paweł Wróbel, Dr Beata Ostachowicz. Photo by Michał Kud

Thus, the results suggest that the trace element metabolism, primarily of rubidium, is impaired in the early stages of obesity. Rats fed a high-calorie diet for seven and a half weeks had significantly higher rubidium levels in all tissues tested in relation to individuals in the control group. This is consistent with other reports, for example, on increased rubidium content in the hair of obese women. The findings give hope that rubidium could become a marker to detect obesity at its early stages and avoid the need for lengthy and costly treatment, which is often ineffective due to the advancement of the disease. However, the researchers are cautious and stress that the results of the animal studies conducted so far will need further experimental verification during clinical trials.
 Pre-election meeting with a candidate for the position of rector
Pre-election meeting with a candidate for the position of rector  Agreement on cooperation with OPAL-RT
Agreement on cooperation with OPAL-RT  Krakow DIANA Accelerator consortium members with an agreement
Krakow DIANA Accelerator consortium members with an agreement  Meeting with the Consul General of Germany
Meeting with the Consul General of Germany  More Academic Sports Championships finals with medals for our students
More Academic Sports Championships finals with medals for our students  Professor Jerzy Lis re-elected as AGH University Rector
Professor Jerzy Lis re-elected as AGH University Rector  Launch of AGH University Student Construction Centre
Launch of AGH University Student Construction Centre  Bronze for our swimmers at Academic Championships
Bronze for our swimmers at Academic Championships